Celiac Disease: When Gluten Free is Not Enough
You’ve probably heard of celiac disease, gluten, and a gluten-free diet. If not, celiac disease is an autoimmune disease that affects 1 in 100 people (1). Gluten is a protein found in wheat, rye, barley, and foods contaminated with these grains. A gluten-free diet avoids all sources of gluten.
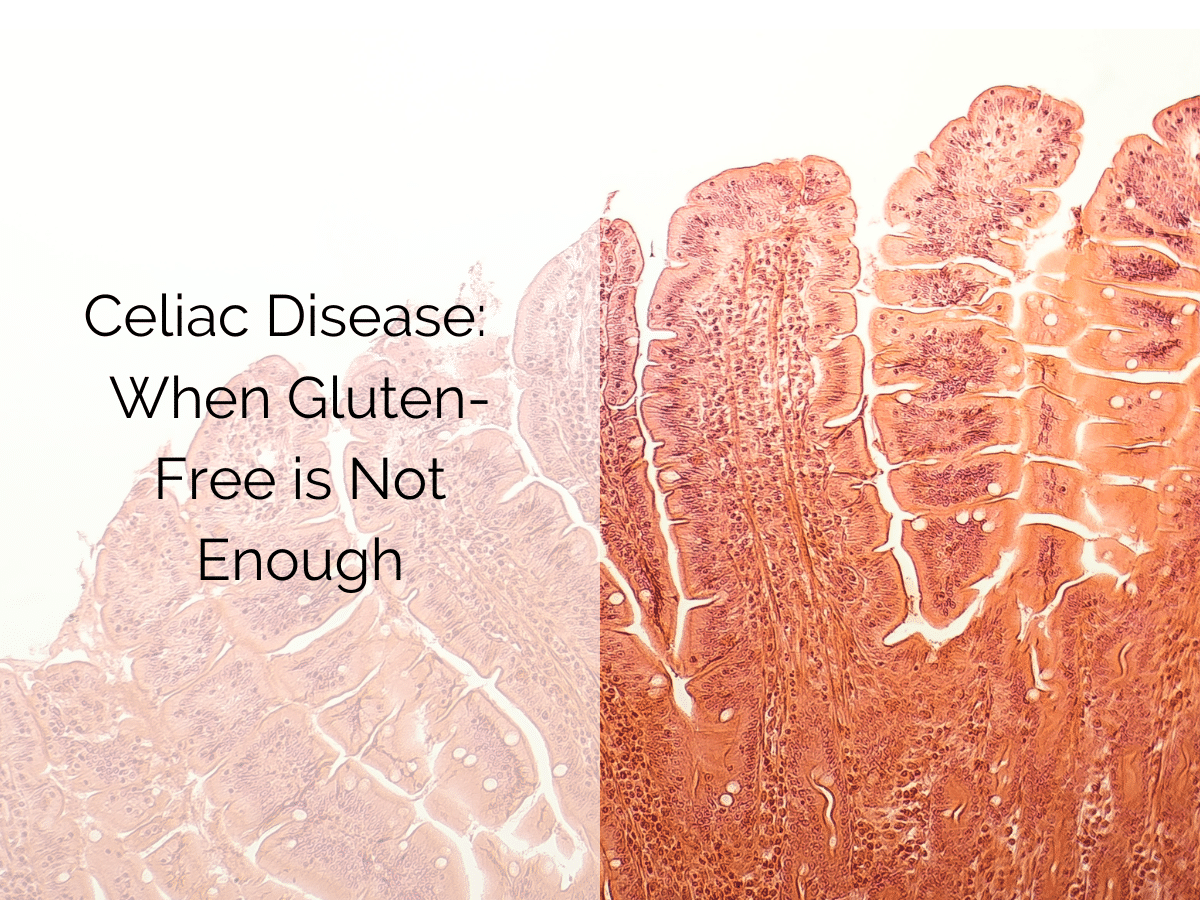
For those with celiac, gluten triggers an immune reaction that damages the villi or the small, finger-like projections that line the small intestine. Healthy villi (pictured) absorb vitamins, minerals, and other nutrients from the food you eat (2).
When damaged, villi flatten reducing the necessary surface area for optimal nutrient absorption. Damaged villi can cause malabsorption and serious nutrient deficiencies.
For most with celiac, twenty parts per million (20 ppm) is considered gluten-free (3). However, research suggests a small group of people react to trace amounts of gluten below the 20 ppm threshold. These people may have refractory celiac disease.
A gluten-free diet is still the only cure for celiac, but what if gluten-free just isn’t enough?
Let’s discuss the next steps to ensure you get your health back on track.
Antibodies and Antibody Testing: A Quick Review
Antibody testing is the first step to diagnosing celiac disease (2). Antibodies are produced by the immune system in response to something that the body perceives as a threat (gluten). People with celiac who eat gluten have higher than normal levels of certain antibodies in their blood.
Antibody Testing
For antibody testing to be accurate, gluten (the threat) must be regularly eaten (2). If you suspect celiac disease, it is important to have antibody testing done before you start a gluten-free diet. A simple blood test looks for elevated levels of these antibodies.
- Anti-tissue transglutaminase
- Anti-deamidated gliadin peptides
If you are positive for these antibodies, discuss further testing with your practitioner. An endoscopy is still the gold standard for diagnosing celiac disease (2).
Newly Diagnosed
If you have a new diagnosis, the goal is that your antibody numbers consistently go down or improve (2). Eventually, you want a negative result. A negative result means that your diet does not have enough gluten to cause an immune response in your small intestine.
Annual Antibody Testing: A Gluten-Free Report Card
After achieving a negative antibody result and your symptoms have subsided, you are successfully living with celiac. Woohoo!
But that doesn’t mean you should stop getting annual antibody testing (2). Antibody testing for celiac is a non-invasive way to gauge gluten exposure and intestinal health.
Still Being Exposed to Gluten: Now What?
If you are still being exposed to gluten, it’s time to take a deep dive. Scrutinize your diet, medications, hygiene, dining out habits, plus food preparation and handling practices.
Diet, Medication, and Hygiene:
Gluten likes to hide. Not to mention, ingredients can change without notice. My top 5 reminders for avoiding gluten.
- Recheck food labels.
- Be cautious with products containing the statement, “manufactured in a plant that also produces wheat.”
- Recheck all over-the-counter and prescription medications to ensure they do not contain gluten.
- Ensure oats are certified gluten-free. Consider eliminating even gluten-free oats. Not everyone can tolerate oats.
- Recheck the labels of anything that comes in contact with the mouth: lickable envelops and stamps, lipstick (balm and gloss), play-doh.
Dining Out:
- Do your homework before you go. Visit the website for a menu or call the manager to discuss gluten-free options.
- Eat simple foods prepared without added breading, sauces, marinades, and/or gravies will be the safest choices.
- Tell your server you need a gluten-free meal. If you have celiac, gluten-containing foods, i.e. croutons and buns, cannot simply be removed after being placed on your plate.
- Use a Nima. Nima is a portable gluten tester that allows consumers to test meals for gluten in about 2 minutes.
- Use gluten-free apps such as Nima or Find Me Gluten Free. These apps are the Yelps of the gluten-free world.
- Tolerase G, an enzyme, has been shown to break down glutenin and gliadin proteins in the stomach and significantly reduce the amount of gluten reaching the small intestine (4). Wheat Rescue is my go-to when eating out or in unfamiliar environments. This product will only help with tiny amounts of wheat, so always continue to eat gluten-free. When you order directly from Microbiome Labs, use the coupon code HONEST to get 10% off Wheat Rescue.
Food Preparation and Handling:
- Clean your kitchen like you’ve never cleaned it before. And repeat if you share a kitchen with gluten eaters. Gluten lurks in the toaster, toaster oven, microwave, air fryer, waffle iron, colander, cutting board, oven, counter, kitchen sponge, dish towels, potholders, and more!
- Make designated gluten-free areas. I recommend kitchen counter space and storage.
- Condiments. Avoid “double-dipping” in shared condiment jars. I like squeeze jars best!
- Utensils and cookware. Toss those with scratches or compromised surfaces. Be mindful of old pans with deep crevices. Stainless steel and glass surfaces are your best bet. Plastic is easily scratched making it an easy spot for gluten to hide.
- Color code cutting boards, colanders, and other shared tools. Many kitchen tools are consistently available in red. Whatever you decide, be consistent.
- Make it difficult for gluten to enter your food chain. Provide a barrier between your gluten-free food and a potentially contaminated area. Use a paper plate, toaster bags, parchment paper, or aluminum foil.
Refractory Celiac Disease
Still, getting a positive antibody test after you’ve taken a deep dive into diet and lifestyle? You may need to consider refractory celiac disease.
Refractory celiac disease is defined as ongoing persistent symptoms, elevated antibodies, or small intestinal damage even after following a strict gluten-free diet for 6 to 12 months (3). If you fall into this small group, a Gluten Contamination Elimination Diet (GCED) might be the answer.
The GCED eliminates any possible source of gluten exposure. The guidance of a knowledgeable dietitian is essential to ensure this diet is customized for you. The good news is that most of the patients in a 2013 study were able to eventually return to a “traditional” gluten-free diet (5).
Final Thoughts
Gluten triggers an immune reaction that causes damage to the villi that line the small intestine in people with celiac.
Antibody testing is the first step to diagnosing celiac disease. Antibody testing is a non-invasive way to gauge gluten exposure and the health of your small intestine health.
A positive antibody test means it’s time to carefully review your diet and lifestyle.
If you’ve done your homework and still test positive for celiac antibodies, you should discuss refractory celiac disease and a Gluten Contamination Elimination Diet (GCED) with your medical practitioner. The guidance of a knowledgeable dietitian is essential to ensure this diet is customized for you.
To learn more about optimizing your digestive health, book a free discovery call with a gut health nutritionist.
All Our Blogs


Surviving the Holiday Season: A Balanced Approach
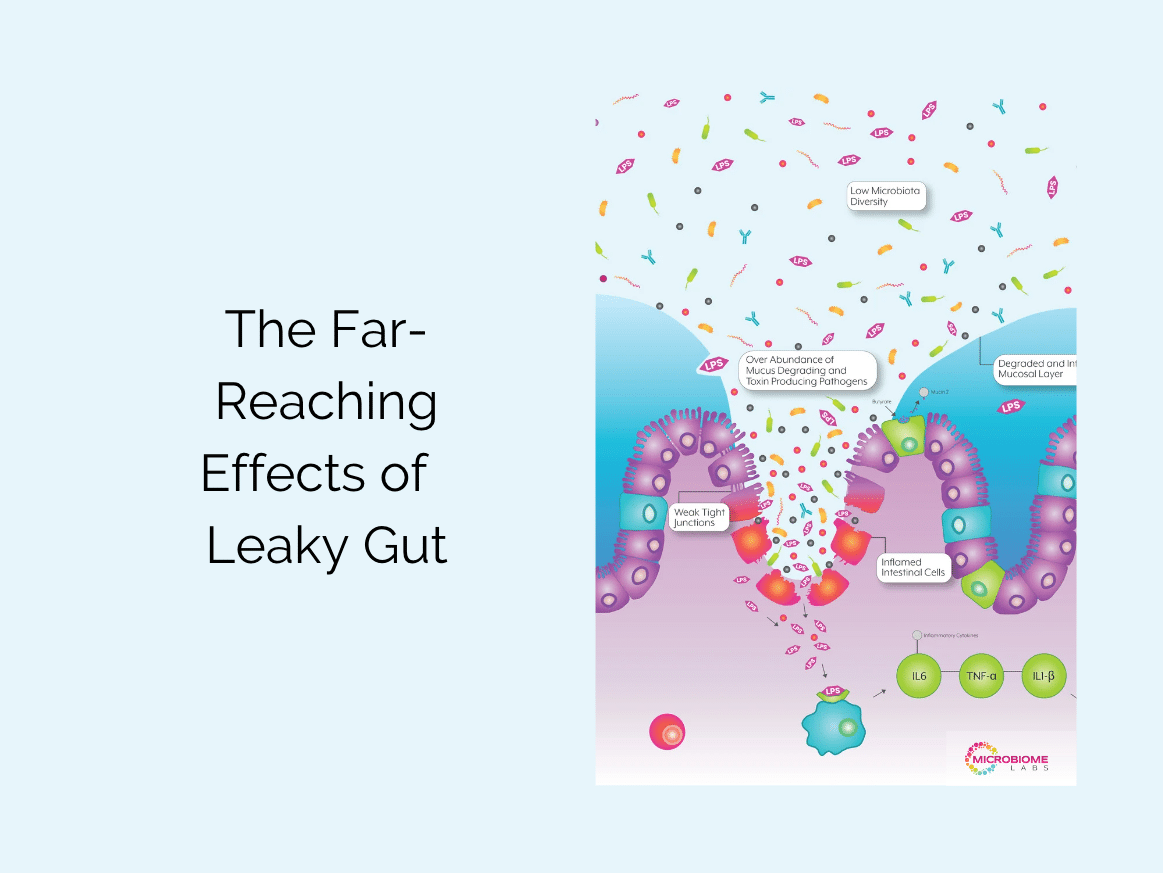
The Far-Reaching Effects of Leaky Gut
The Skinny on Non-Caloric Sweeteners

Fermented Foods for a Healthy Gut & More